The Ultimate Running Injury Guide: Runners Knee (PFPS)
What is PFPS?
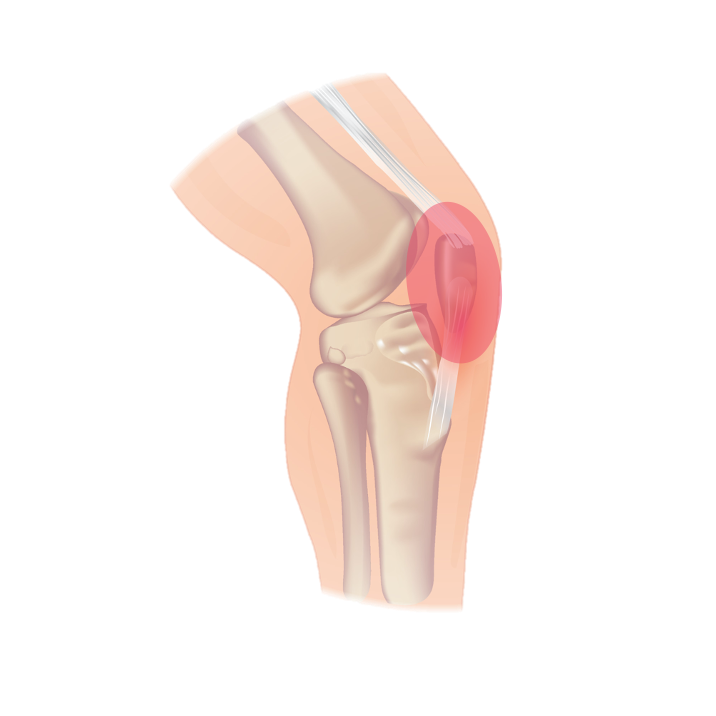
Runner's knee, also known as patellofemoral pain syndrome (PFPS), is the most common running injury and is characterized by gradual onset pain localized to the front of the knee. The pain is felt around or behind the patellofemoral joint (PFJ) which is the connection between the patella and the femur. This pain is often associated with PFJ loading activities such as squats, stairs, and running.
Although various factors such as misalignment, patellar maltracking, weak muscles, and abnormal movement patterns have been suggested as possible causes of PFPS, there is little evidence to show a clear link between these factors and the symptoms experienced. Therefore, diagnosis is based on a cluster of signs and symptoms after ruling out other potential diagnoses.
Signs & Symptoms
The most common symptom of PFPS is vague frontal knee pain, which is usually felt around or behind the patella. Other symptoms may include tenderness and pain while performing activities that load the PFJ, such as squats, stairs, or running. People with PFPS often experience pain and stiffness associated with prolonged periods of rest or sitting.
In terms of running, knee pain may also be felt during and after a run, especially at high speeds and while running uphill or downhill.
Risk factors & Related Conditions
Several factors may increase the risk of developing PFPS. These include isometric quad weakness (however, this is not established in runners) and hip musculature weakness, including abduction, external rotation, and extension of the hip. Note that hip weakness may be a consequence of pain which can make determining cause and effect difficult.
Training errors, such as increasing training volume, frequency or intensity too quickly, can also increase the risk of PFPS and is often the most present risk factor.
Many conditions can also mimic the symptoms of PFPS, and ruling out these other conditions is essential. Some of the conditions that are similar to PFPS include quad/patellar tendinopathy, Osgood-Schlatter disease, Sinding-Larsen-Johansson (SLJ) syndrome, knee osteoarthritis, bursitis, and iliotibial band syndrome (ITBS).
Each of these conditions has its unique set of signs and symptoms, and correct diagnosis is crucial for proper treatment. For more information on these similar conditions and their signs and symptoms, here’s a video addressing the conditions in detail.
How long until you recover? (Prognosis)
According to research, about 30% of people with PFPS experience improvement in their symptoms within three months, and 50-75% can expect long-term improvement lasting several years.
About 25% of people with PFPS that see improvement expect complete resolution of symptoms long-term, but 70-90% will continue to have recurrent symptoms.
It is important to note that earlier treatment leads to better outcomes, so it's best to seek help as soon as you experience any of the symptoms of PFPS.
Treatment
We will break treatment into 3 categories.
“Yes” treatments have strong research backing, “Maybe” treatments lack significant support from the research, and “No” treatments are not recommended by research.
Yes
First-line treatment options for runner's knee are:
1) Education: Decreasing running speed, avoiding hills and splitting total weekly distance into more frequent but shorter sessions
2) Load Management: Including the volume, frequency, and intensity of PFJ loading activities like running and weightlifting
3) Therapeutic Exercise: A combination of hip and knee exercises tend to have better results
4) Taping: Often helpful in the short-term (days to weeks)
5) Over-the-counter orthotics: Can be helpful for those with increased pronation in the short-term (days to weeks)
6) Some combination of the above!
Maybe
1) Gait Retraining: Gait retraining involves making changes to how a person runs. These changes are often small and temporary. Retraining tips include running softer, moving from a rear foot strike to a midfoot or forefoot strike, decreasing hip adduction, and increasing cadence.
2) Blood Flow Restriction: Used in combination with the therapeutic exercise intervention.
3) Lower Profile Footwear: Maximalist footwear can increase PFJ contact force by roughly 20% per step and 10% per mile compared with traditional shoes.
No
1) Sleeves / Braces
2) Dry Needling / IMS
3) Manual therapy, including lumbar, knee, or patellofemoral manipulation or mobilization
4) Ultrasound
5) Low-level laser therapy
6) Electrical stimulation, including TENs, IFC and NMES
7) Ice
It is not recommended to rely solely on the "educate and wait" approach of avoiding pain-provoking activities, as it is not effective in improving pain and function in the short, medium, or long term.
Surgery is also rarely necessary, and most people with PFPS can manage their symptoms with conservative treatment.
Conclusion
In conclusion, runner's knee, or PFPS, is a common condition that can be well managed with conservative treatment. If you're experiencing any symptoms of PFPS, it's important to seek help from a qualified physiotherapist or healthcare professional to receive a proper diagnosis and treatment plan.
Happy Running!
- Jeremy
Looking for something else?
References
What is PFPS?
Esculier, J.-F., Maggs, K., Maggs, E., & Dubois, B. (2020). A contemporary approach to patellofemoral pain in runners. Journal of Athletic Training, 55(12). https://doi.org/10.4085/1062-6050-0535.19
Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., Lynch, A. D., Snyder-Mackler, L., & McDonough, C. M. (2019). Patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302
Signs & Symptoms
Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., Lynch, A. D., Snyder-Mackler, L., & McDonough, C. M. (2019). Patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302
Risk Factors & Related Conditions
Esculier, J.-F., Maggs, K., Maggs, E., & Dubois, B. (2020). A contemporary approach to patellofemoral pain in runners. Journal of Athletic Training, 55(12). https://doi.org/10.4085/1062-6050-0535.19
Johnson, C. D., Tenforde, A. S., Outerleys, J., Reilly, J., & Davis, I. S. (2020). Impact-related ground reaction forces are more strongly associated with some running injuries than others. The American Journal of Sports Medicine, 48(12), 3072–3080. https://doi.org/10.1177/0363546520950731
Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., Lynch, A. D., Snyder-Mackler, L., & McDonough, C. M. (2019). Patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302
Treatment
Esculier, J.-F., Bouyer, L. J., Dubois, B., Fremont, P., Moore, L., McFadyen, B., & Roy, J.-S. (2018). Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain? A randomised clinical trial. British Journal of Sports Medicine, 52(10), 659–666. https://doi.org/10.1136/bjsports-2016-096988
Esculier, J.-F., Maggs, K., Maggs, E., & Dubois, B. (2020). A contemporary approach to patellofemoral pain in runners. Journal of Athletic Training, 55(12). https://doi.org/10.4085/1062-6050-0535.19
Johnson, C. D., Tenforde, A. S., Outerleys, J., Reilly, J., & Davis, I. S. (2020). Impact-related ground reaction forces are more strongly associated with some running injuries than others. The American Journal of Sports Medicine, 48(12), 3072–3080. https://doi.org/10.1177/0363546520950731
Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., Lynch, A. D., Snyder-Mackler, L., & McDonough, C. M. (2019). Patellofemoral pain. Journal of Orthopaedic & Sports Physical Therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302